-
-
Preventing the Next Pandemic
-
-
-
Lecture II.
-
-
-
Background
-
-
1.1 Preventing the Next Pandemic » What, when and where?
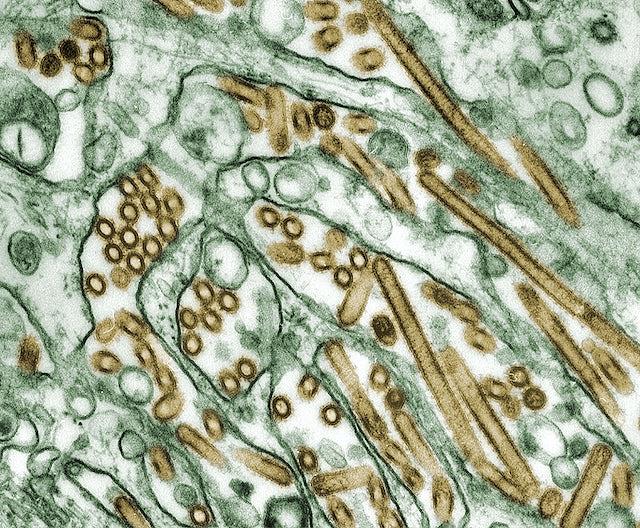
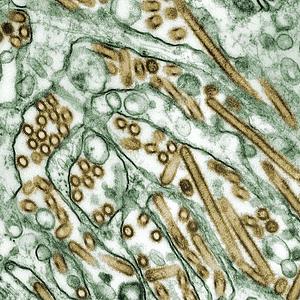
Dr. Lauren Ancel Meyers presented the lectures in this module in September 2019, at the start of flu season in the US and approximately three months before the first cases of COVID-19 were recognized in China. She spoke about predicting the next influenza pandemic, as experts thought that the influenza virus was the most likely source of a global disease outbreak. Coronaviruses generally elicit diseases with relatively mild upper-respiratory tract symptoms, like the common cold. The coronavirus diseases SARS in 2002-2003 and MERS in 2012 were notable exceptions, as patients experienced severe symptoms. SARS and MERS outbreaks were quickly contained despite their deadliness, killing 10% and 30% of infected patients, respectively. The 2009 H1N1 influenza pandemic that spread around the world was more severe and thus, as Dr. Meyers explains, influenza virus was - and is - a likely candidate to start a pandemic.
The very nature of a pandemic necessitates that the disease-causing pathogen is relatively "new" or unknown from the perspective of our immune systems. Predicting how something new and different will behave has enormous challenges. Experts rely on the patterns of past pandemics to predict what will happen during novel outbreaks. Dr. Meyers and her colleagues have developed computational models and prediction methods based on past influenza pandemics to forecast certain features of future pandemics. With more data, those computational models can be refined and deployed to predict not only the course COVID-19 but also to generate better predictions about future threats.
But why predict a pandemic if we can't cure the disease? Prediction can help officials allocate hospital resources, equipment and supplies, and staff, or make decisions about school closures, mask mandates, or other public health interventions. Dr. Meyers and her colleagues work with government officials and health care experts to simulate pandemics and find out how different preparations or interventions affect outcomes. For example, their models allow city officials to ask what will happen if they close schools on day 3 of an outbreak versus waiting until day 4 and allow hospital systems to ask how many respiratory ventilators should each hospital have so that they can meet anticipated needs and be deployed across a region as quickly as possible.